Rural Pharmacy Health Initiative
An initiative contributing to the growth of the rural health care workforce, working with community partners to expand upon team-based and collaborative health care innovations
Launched by the UNC Eshelman School of Pharmacy with Carolina Across 100
Why Does this Work Matter?
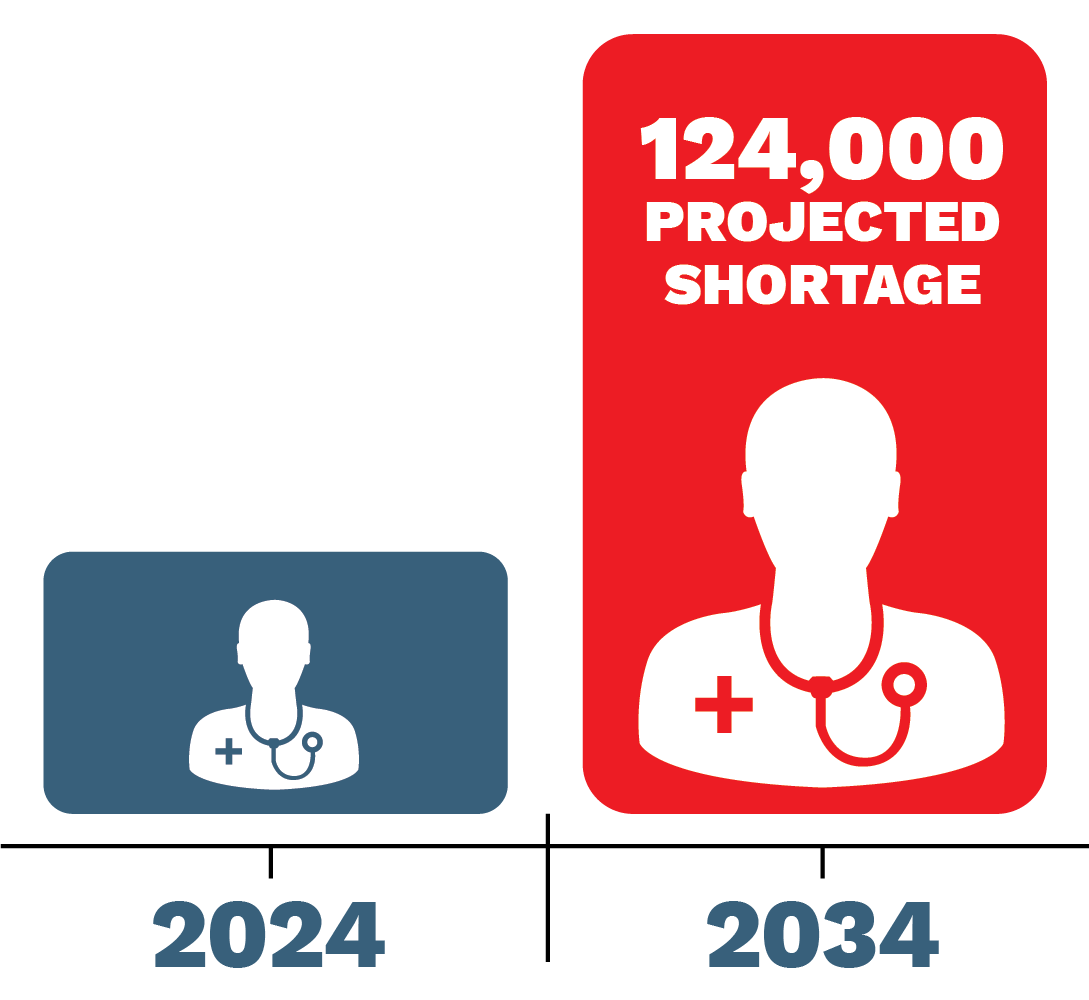
Better access to primary care is associated with reduced health care disparities and better health outcomes across socioeconomic circumstances, yet rural communities struggle to recruit and retain health care professionals. The shortage of primary care providers in the U.S. is significant, with an anticipated shortage of up to 124,000 physicians over the next decade.
In the next decade, the U.S. will have an anticipated shortage of up to 124,000 primary care providers.
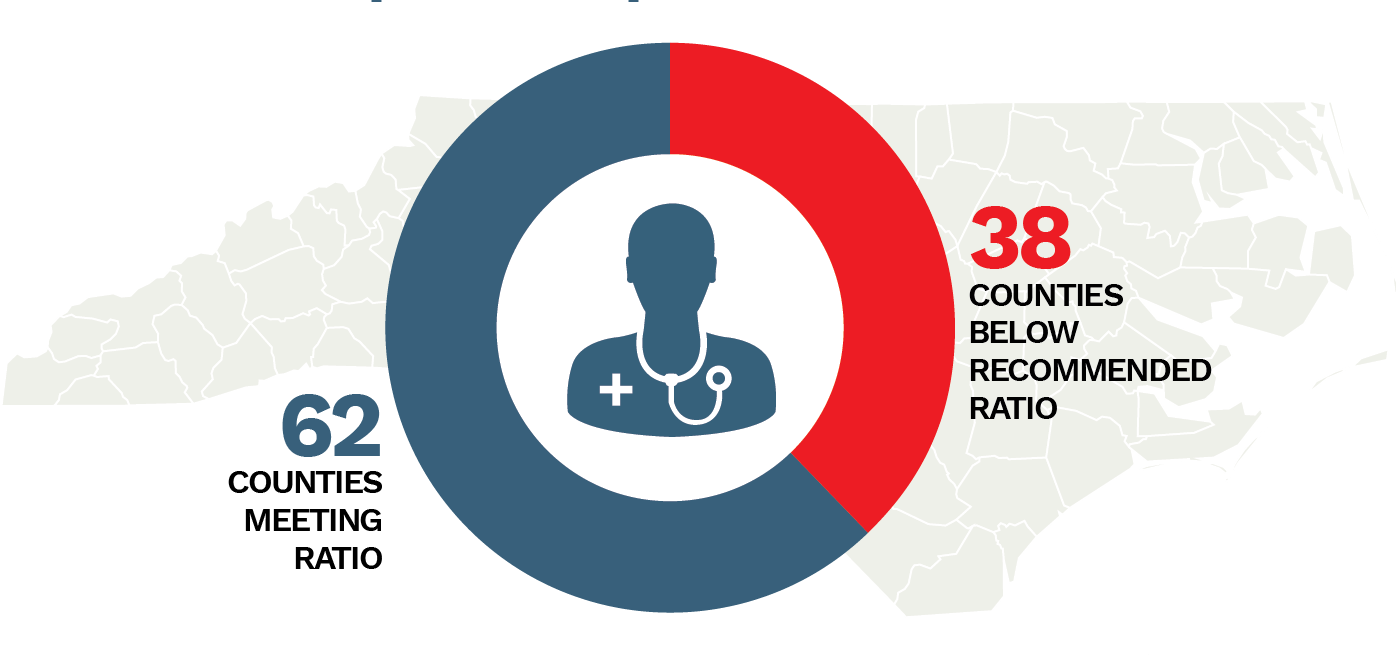
These shortages are most pronounced in rural areas, including North Carolina’s 78 rural counties, and are heightened by an aging and growing population. Thirty-eight counties in North Carolina do not meet the recommended ratio of one primary care provider per 1,500 residents and access to medical services may be limited by geography, distance, and economic challenges. Health care workforce shortages result in unmet health care needs, delays in receiving care, forgoing preventive care, preventable hospitalizations and death. In support of increasing access to primary care, team-based and interprofessional health care approaches have been leveraged as one way to expand access to much needed care. Pharmacists are often an integral, yet underutilized, member of the health care team.
38 counties in North Carolina do not meet the recommended ratio of one primary care provider per 1,500 residents.
Approximately 50-75% of patients do not take their medications as prescribed.
Non-adherence has been shown to cost $100 billion each year in excess hospitalizations.
Community based pharmacy an untapped resource
As one of the most accessible health care providers in rural communities, pharmacists are well positioned to fill gaps in care. The state of North Carolina has at least one pharmacy in all 100 counties, and the average patient visits a pharmacy nearly 10 times more often than a primary care provider. Pharmacists often build strong relationships with patients and provide value beyond dispensing medications. Collaborating with medical teams, pharmacists play an essential role in optimizing medication therapy and serving as a liaison between the patient, their primary care provider and other essential members of the health care team. Pharmacists ensure medication therapy is safe, effective, affordable and accessible. They can also play a key role in adherence to medications, particularly in the management of chronic diseases such as diabetes, hypertension, congestive heart failure and respiratory diseases. These enhanced pharmacy services – medication management, counseling and more – translate directly into improved patient health, better-coordinated care, and reduced costs, as well as improved well-being for the care team.
Pharmacist transitions of care services provided from hospital to the community pharmacy have been shown to reduce rehospitalization rates for Seniors and reduce overall healthcare costs.
Rural Pharmacy Health Initiative
Carolina Across 100 is supporting the further expansion of the rural hubs framework. Led by the UNC Eshelman School of Pharmacy and its Rural Pharmacy Health Initiative, and in collaboration with cross-sector community partners, this partnership will add additional support to:
- Improving and expanding efforts to inspire, recruit and train the future health care workforce in rural regions of North Carolina
- Establish a rural internship infrastructure to increase engagement of pharmacy students in rural North Carolina
- Expand upon successful collaborative practice initiatives that engage pharmacists in team-based care to increase patient access to high quality medication optimization services and contribute to improving health outcomes.
The Rural Pharmacy Health Initiative is a unique educational program that stretches across North Carolina to forge a path for better health for medically underserved communities. The establishment and support of a rural hub in Northeastern North Carolina in partnership with Roanoke Chowan Community Health Center and the local community, will focus upon addressing rural health care provider shortages. A series of internships for high school students and current pharmacy students will be established to build a more cohesive pathway for future rural practice opportunities. Working collaboratively with two other rural hubs, funded through a grant from The Duke Endowment, also located in Eastern North Carolina, this initiative will provide much needed infrastructure to build and deliver innovative models of practice, and deliver high-quality care for medically underserved communities. These rural hubs will provide unique educational opportunities to develop the pharmacist workforce Eastern North Carolina needs while at the same time serving as an important resource to patients.
Counties Involved